New WHO/Europe strategy urges countries to urgently address gaps in pandemic monitoring and response to avoid preventable deaths and severe disruptions
Statement by WHO Regional Director for Europe, Dr Hans Henri P. Kluge
At this time last year, I spoke to you about a new wave of COVID-19 sweeping across the Region, driven by the Delta variant amid the lifting of restrictions and increased social mixing.
It’s now abundantly clear we’re in a similar situation to last summer – only this time the ongoing COVID-19 wave is being propelled by sub-lineages of the Omicron variant, notably BA.2 and BA.5, with each dominant sub-lineage of Omicron showing clear transmission advantages over the previously circulating viruses. With rising cases we’re also seeing a rise in hospitalisations, which are only set to increase further in the autumn and winter months as schools re-open, people return from holidays, and social mixing moves indoors with the onset of colder weather. This forecast presents a huge challenge to the health workforce in country after country, already under enormous pressure dealing with unrelenting crises since 2020.
Read also
Consider the current situation: The European Region has seen a tripling of new COVID-19 cases over the past six weeks, with close to three million new cases reported last week, accounting for nearly half of all new cases globally. While hospitalisation rates due to COVID-19 have doubled in the same period, ICU admissions have so far remained relatively low. However, as infection rates in older groups continue to rise, Europe is still seeing close to 3,000 people die of COVID-19 every week.
These numbers paint a picture of the recent past. Looking to and preparing for the future is much more difficult yet must be urgently tackled. That’s why today, WHO/Europe is releasing its autumn/winter strategy for COVID-19 and other respiratory viruses – to help prepare for the coming waves of infection. Waiting for the autumn to act will be too late.
The strategy calls on countries to re-launch mitigation efforts and be ready to respond to an increased burden on their healthcare systems. The consistent application of the following five pandemic stabilisers will continue to be critical to protect people this autumn and winter:
- Increasing vaccine uptake in the general population,
- Administering a second booster dose to immunocompromised people aged 5 and above and their close contacts, and consider offering a second booster to specific at-risk groups, at least three months after their last dose,
- Promoting mask-wearing indoors and on public transportation,
- Ventilating crowded and public spaces (such as schools, offices, and public transport), and
- Applying rigorous therapeutic protocols for those at risk of severe disease.
These stabilisers should be underpinned by:
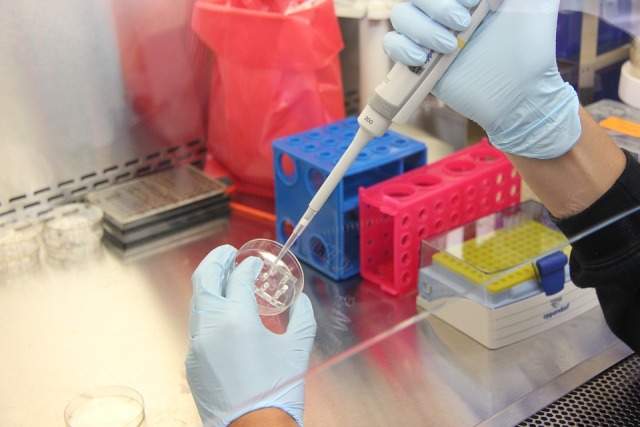
- Strengthening laboratory capacities to ensure reliable rapid diagnostic SARS-CoV-2 detection and tracking of variants, complemented by continued population use of rapid diagnostic testing,
- Integrating population-based surveillance systems for influenza, SARS-CoV-2, and other respiratory viruses to monitor the spread and intensity of respiratory viruses,
- Prioritising contact tracing and quarantine based on WHO recommendations for individuals, high-risk settings, and situations of concern,
- Promoting informed individual choices around protection measures including respiratory hygiene, mask-wearing, ventilation, handwashing, and vaccination, and
- Strengthening infection control practices in all healthcare and care settings, as well as in the community.
COVID-19 remains a nasty and potentially deadly illness. Just two weeks ago, I was struck down with the virus for the first time, and it knocked me off my feet. I spent three awful days and nights with high fever, shivers, and shortness of breath. I can only imagine how bad it would have been had I not been fully vaccinated and received my additional dose. I recovered at home, in isolation, with my family nearby to keep an eye on me. I didn’t need hospitalisation or treatment. The vaccine-induced antibodies in my immune system set to work and fought off the infection. My advice to everyone who gets infected is to take it easy. Just because your symptoms have ceased does not necessarily mean you have fully recovered. And when you do return to your normal routine, do it gradually, if at all possible.
More than two years into the pandemic, we’re all aware of the tools we have to keep ourselves safe, assess our level of risk, and take the necessary steps to protect others if we get infected. Make your own informed decisions. Just because a mask isn’t mandated, doesn’t mean it’s prohibited.
Repeated infections with SARS-CoV-2 are occurring due to the continued evolution of the virus, and each new infection could lead to long COVID. In the United Kingdom alone, for example, an estimated two million people – 3% of the population – suffer from long COVID. Much more needs to be done to establish best practices for the detection, treatment, and rehabilitation of long COVID patients. I continue to call on countries to recognise the problem and invest in the research needed to respond to COVID-19’s shadow pandemic.
To reiterate: my message to governments and health authorities is to act now to prepare for the coming months. Right now, the Southern Hemisphere, where it is winter, is experiencing a very active influenza season, which, along with COVID-19, is putting a continued strain on health systems. We are likely to see a similar scenario in the Northern Hemisphere come autumn and leading into winter. If health authorities act now, they can help reduce the anticipated disruptions to society, including health worker absences and overburdened health systems, struggling businesses and travel chaos.
Our health systems and society at large must continue to adapt in our collective response to this virus – and any future variants of concern. We must continue to do all we can to protect those at most risk. This means we must continue to monitor and track the evolution of SARS-CoV-2, which remains a highly unpredictable virus. Yet most countries in the European Region have stopped or greatly reduced COVID-19 surveillance, creating a dangerous blind spot in our knowledge of how the virus is evolving.
I therefore urge all countries to continue to strengthen COVID-19 surveillance as part of wider resilient population-based surveillance for respiratory viruses and get ready for the autumn. Knowledge has been and remains a vital tool against the virus. Let’s not throw that away.